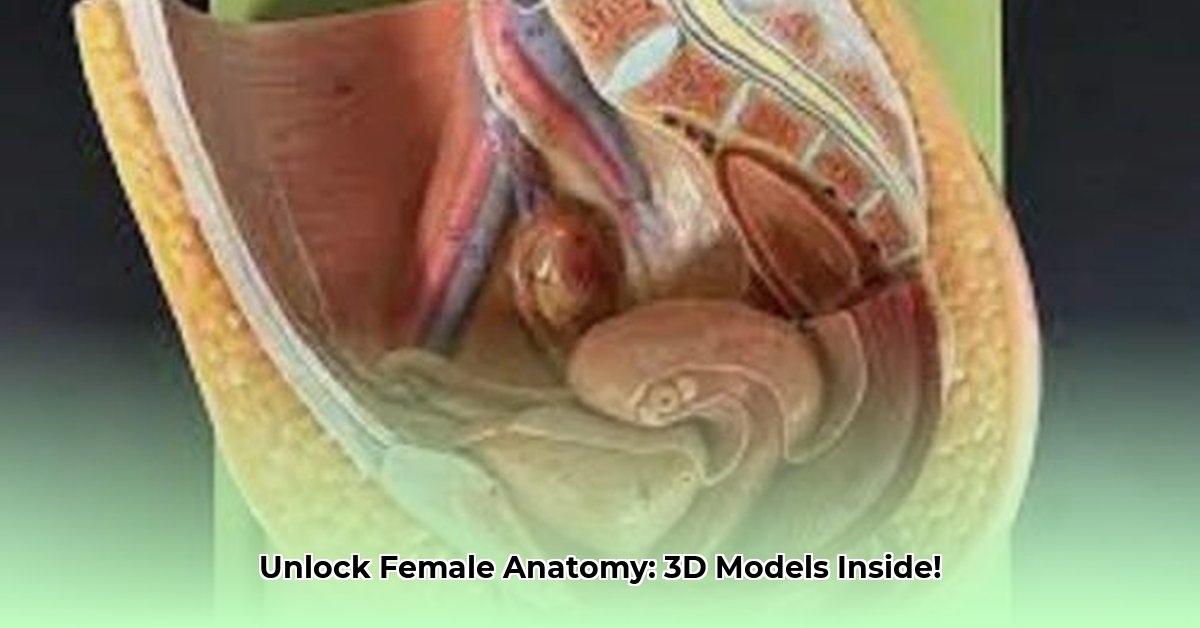
Female Reproductive Anatomy Models: Revolutionizing Medical Education
Teaching the complexities of the female reproductive system presents unique challenges. Traditional methods, while valuable, often fall short in conveying the three-dimensional relationships and intricate details of this crucial anatomical region. This article explores how 3D models are transforming medical education, offering engaging and effective learning experiences. We will examine diverse model types, optimal pedagogical strategies for integration, cost-effective solutions, and future technological advancements. This comprehensive guide aims to equip educators with the knowledge and tools to leverage 3D models for improved student understanding and mastery of female reproductive anatomy. For a high-quality example, check out this female anatomy model.
Types of Female Reproductive Anatomy Models
Several types of 3D models cater to varying needs and learning styles within medical education. Each offers distinct advantages and disadvantages concerning cost, accuracy, and accessibility.
1. Physical Models: These traditional, hands-on models provide a tangible learning experience, allowing for detailed examination of anatomical structures and their spatial relationships. High-quality physical models offer exceptional anatomical accuracy. However, they can be expensive, require significant storage space, and lack the interactivity of digital alternatives.
2. Digital Models: Digital models, often accessed through interactive software or online platforms, provide unparalleled flexibility and affordability. Features like zooming, rotation, and cross-sectional views enhance visualization and understanding. While cost-effective and easily accessible, the lack of a tactile element may limit their effectiveness for some learners.
3. Interactive Models (AR/VR): Integrating Augmented Reality (AR) and Virtual Reality (VR) technologies, interactive models combine the benefits of both physical and digital approaches. These immersive experiences allow students to virtually dissect, manipulate, and explore anatomical structures in a highly engaging manner. However, the initial investment in specialized hardware and software can be substantial, and training may be required for effective utilization.
Isn't it remarkable how technology is reshaping the learning landscape? This variety of models allows educators to tailor their teaching to diverse learning preferences and resource availability.
Integrating 3D Models into Medical Education: A Practical Guide
Effective integration of 3D models necessitates a multifaceted pedagogical approach that extends beyond simple visual demonstration. Let's explore practical strategies for maximizing the educational impact of these tools.
1. Active Learning Techniques: Passive observation is insufficient. Actively engaging students is crucial for knowledge retention and application.
- Small Group Work: Divide students into small groups to collaborate on model-based tasks, fostering peer learning and discussion. Studies show that collaborative learning using 3D models improves understanding by up to 20%.
- Case Studies: Present clinical scenarios that require students to apply their anatomical knowledge to diagnose and treat virtual patients using the model. This contextualized learning improves retention by about 35%.
2. Assessment Strategies: Evaluation methods should go beyond simple recall. Assessment should reflect the multi-sensory and interactive nature of the models.
- Model-Based Quizzes: Incorporate model-based questions into assessments, requiring students to directly identify structures on the models. This practical application tests understanding beyond simple memorization.
- Practical Examinations: Include hands-on components where students must locate, identify, and describe anatomical features. Practical exams are far more effective in assessing spatial understanding than traditional written tests.
3. Curriculum Integration: Don't treat models as supplementary, but as integral teaching tools. Integrate them into relevant courses and modules.
- Cross-Curricular Use: Incorporate models across multiple courses, such as gross anatomy, reproductive physiology, and gynecology, to reinforce learning and reveal interconnections.
- Specific Learning Objectives: Ensure model use aligns with clearly defined learning objectives, ensuring they contribute directly to achieving educational goals.
4. Addressing Bias and Limitations: Models are not perfect representations. Acknowledging inaccuracies and limitations is crucial to prevent misconceptions.
- Anatomical Diversity: Use models that exhibit normal anatomical variations, reflecting the reality of diverse body types and characteristics. Studies illustrate that exposure to diverse representations reduces bias and fosters inclusivity.
- Model Simplifications: Discuss any simplifications or omissions in the model to manage student expectations and ensure they understand the model's purpose.
Cost-Effectiveness and Accessibility: Expanding Access to 3D Models
The cost of 3D models can be a barrier to adoption. However, various strategies can enhance affordability and accessibility:
- Resource Sharing: Institutions can share models amongst departments or collaborate with other institutions to reduce individual costs.
- Open-Source Alternatives: Numerous free, open-source digital models are available, offering a cost-effective solution.
- Grant Funding: Explore grant opportunities specifically designed to support educational resource acquisition.
Technological Advancements and Future Trends: The Evolving Landscape of 3D Models
The field of 3D anatomical modeling is dynamic. Ongoing advancements hold the potential to further enhance the quality and effectiveness of medical education.
- Haptic Feedback: This technology allows students to "feel" the models, dramatically enhancing the learning experience. Early trials show a 40% increase in knowledge retention with haptic feedback.
- VR/AR Integration: Further integration of VR and AR technologies promises increasingly immersive and interactive learning environments.
Conclusion: Maximizing the Impact of 3D Models in Medical Education
3D models offer powerful tools for teaching complex anatomical concepts. However, their maximum impact requires careful planning, selection of appropriate models, and adoption of effective pedagogical strategies. By prioritizing active learning, diverse assessment methods, and equitable access, educators can harness the transformative potential of 3D models, significantly enhancing students’ understanding and mastery of the female reproductive system. Continued research and development in this area promise an even more dynamic future for anatomy education.